What is an intrauterine device?
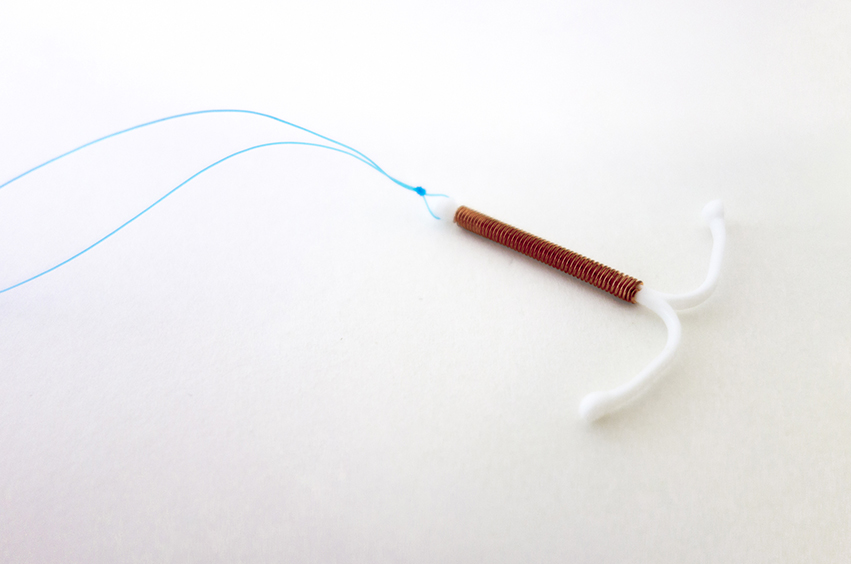
An intrauterine device (IUD) is a type of birth control. It is a small, T-shaped device that a doctor or nurse puts in a uterus by going through the vagina and cervix. These devices are made of flexible plastic and have two thin plastic strings that hang out of the cervix. They are very small – a little more than 1 inch (2.5 cm) in width and length.
An IUD is one of the safest, most effective methods for preventing pregnancy. It is a good choice for women or teens who do not want to get pregnant for at least one year.
Some women use IUDs for reasons other than birth control. For example, one type of IUD can be used to treat heavy, painful periods. The other type can be used to prevent pregnancy if it is put in within five days after a woman has sex without birth control. This is known as “emergency contraception.”
What are the different types of IUDs?
Two types of IUDs are available in the United States. One type releases copper, and the other type releases the hormone progestin.
- Copper-containing IUD – Paragard is the only copper-containing IUD. It is can stay in the uterus for up to 10 years to prevent pregnancy. Some women who use it gain weight or experience longer periods than they had before insertion of the IUD. Paragard also can be used for emergency contraception.
- Progestin-releasing IUD – The four available progestin-releasing IUDs are Mirena, Kyleena, Skyla, and Liletta. Mirena and Kyleena can stay in a uterus for up to five years to prevent pregnancy. Liletta can stay in place for up to four years, while Skyla can stay in place for up to three years. Many women who use progestin-releasing IUDs have lighter, less painful periods than they had before the IUD. Some women stop menstruating altogether, but this is not harmful and does not need to be treated. Regular periods return when the device is taken out.
Other types of IUDs are available outside of the U.S.
What are the benefits of using an IUD?
The benefits of using an IUD include:
- IUDs are effective. Fewer than 1 in 100 women who use these devices get pregnant during the first year of using them.
- Does not rely on remembering to do anything or take any birth control medicines on a regular basis.
- IUDs have few side effects.
- IUDs do not contain estrogen, a hormone that some women can’t or don’t want to take.
- IUDs are easily taken out and do not prevent pregnancy after removal.
- Using an IUD for several years is more cost-effective than many other types of birth control. Insertion of the device is the only cost.
- Using an IUD lowers risk of cervical cancer, according to studies.
What are the downsides of an IUD?
The downsides of an IUD include:
- Unlike condoms, an IUD does not protect against sexually transmitted diseases or STDs. To prevent infections, use condoms.
- The initial cost is higher than the cost of other methods; however, the only cost is insertion and most are covered by insurance.
- Only a doctor or nurse can insert or remove an IUD.
You should not get an IUD if you recently had an infection that spread to your uterus and other nearby organs, called a “pelvic infection.” STDs such as chlamydia and gonorrhea can cause pelvic infections.
Which type of IUD is best?
A doctor can help choose the right IUD for each patient. Paragard might be a good choice if the patient:
- Wants or needs to avoid hormones.
- Wants to avoid big changes in menstruation, such not having any periods or bleeding or unexpected spotting. However, Paragard may make periods heavier and more painful.
- Wants birth control for up to 10 years.
Mirena, Kyleena, Skyla, or Liletta might be a good choice for patients who: - Have heavy, painful periods. These IUDs can make periods lighter and less painful.
- Want birth control for up to five years, depending on which device is chosen.
Does it hurt to have an IUD put in?
Most patients will likely feel some discomfort and slight cramping after the nurse or doctor puts in the IUD. Women who have not had a baby often feel more discomfort than women who have had a baby. The cramps generally go away within a day. Over-the-counter pain medicines like ibuprofen (sample brand names: Advil, Motrin) or naproxen (sample brand name: Aleve) can help cramps go away more quickly.
After the IUD is in place, the patient should not be able to feel it.
When should an IUD user see a doctor?
Patients should see a doctor or nurse right away if the follow occurs:
- Bad pain in the lower belly
- Period is late or very different from normal with Paragard. (Periods may be very light or not occur at all with Mirena, Kyleena, Skyla, or Liletta.)
- Cannot feel the string of the IUD or if the string seems shorter than usual
- IUD seems to have moved or fallen out
- Sex with someone who has or might have an STD, or if the patient suspects he or she has an STD
- Unexplained fever
This topic retrieved from UpToDate on: Nov 21, 2018.

